Parkinson's Disease: How could gene and cell therapy help?
Estamos presentemente a traduzir e a actualizar este material na sua língua. Uma versão actualizada deste conteúdo em inglês pode ser encontrada em baixo.
Parkinson's disease affects millions of people worldwide. Although the symptoms can be treated, there is no known cure. Scientists are investigating how regenerative medicine and stem cell science could be used to better understand, and then treat or prevent, the disease itself.
What do we know?
Parkinson’s disease (PD) is a common incurable condition affecting about 1 in 800 people. The average age of onset is 70 years. The condition affects many areas of the brain, and even the gut. In most cases, we do not know why it occurs (so-called idiopathic PD). However, a major problem is the loss of brain cells releasing the chemical dopamine in one specific part of the brain. This causes problems with movement and thinking. These symptoms can be treated with a number of dopaminergic (dopamine-related) drugs, which greatly help in early stages of disease. However, over time, side effects occur with these drugs. As symptoms progress, more aggressive treatments are sometimes needed, including the implantation of a deep brain stimulation device.
What are researchers working on?
There are two main areas of research in PD. The first is trying to understand what causes the disease. This may not be the same in all patients; there are different types of PD, including very rare genetics forms. The second major area is trying to develop better ways to treat PD. This can either be in the form of targeting what goes wrong and then stopping it or slowing it down (so-called disease modifying therapies), or better treatment of symptoms, including dopamine cell transplants and gene therapies. Many of these therapies are now being trialled in patients with PD.
What are the challenges?
The ability to model PD in the lab is a major challenge for several reasons. Humans are the only animal to develop this condition; the condition typically develops late in life; and the reasons why the disease develops are often not clear. Because of this, it is hard to develop cell or animal models which accurately represent the disease. In recent years, taking cells from patients to grow and study in a lab, has proven helpful. Another major challenge is in trialling new therapies in patients with PD. This is because of the wide variety of symptoms and presentations the disease can take. Parkinson’s symptoms change over the course of a day and the condition can evolve very differently between individuals. It is therefore very hard for clinicians to accurately track the progression of the condition.
Introduction to Parkinson's Disease
Parkinson’s Disease (PD) is a common condition, with about 140,000 cases in the UK, and over 10 million cases worldwide. It can affect people at any age, but typically presents at about the age of 70 years old. Younger patients are more likely to have rarer genetic forms of the condition. Men are affected slightly more frequently than women. Some research has made a link with pesticides, while smoking and coffee appear to reduce the risk of getting the disease, though it is not known why.
One of the major problems in people with PD is that they don't have enough of a brain chemical (neurotransmitter) called dopamine in certain parts of the brain. This chemical is produced by cells (dopaminergic cells) in an area of the brain called the substantia nigra. These cells slowly die off in patients with PD.
The substantia nigra is a part of the circuit in the brain that is involved in regulating movement, as well as mood and decision-making. When about 50% of these dopaminergic cells have been lost, leading to less dopamine in the circuit, patients start to experience the motor symptoms of PD. The characteristic motor features of PD consist of slowness of movement, a tremor, stiffness, a quiet voice and a stooped, shuffling walk. When symptoms begin, one side of the body is typically more affected than the other.
However, it is not only dopamine, or the cells in the substantia nigra, which are affected by the condition. Many other types of nerve cells are affected, and this can lead to non-motor symptoms including a loss of a sense of smell, constipation, acting out their dreams (REM sleep behavioural disorder), some loss of motivation, and low mood. These can occur before the motor symptoms, and have now been termed prodromal or premotor PD.
Alongside the loss of the dopaminergic cells, PD can normally only be confirmed at autopsy. This confirmation relies on the identification of a protein in the brain called alpha-synuclein. In PD, this protein behaves abnormally and ‘clumps’, forming structures called Lewy bodies. Exactly how this protein starts to accumulate and cause problems is unknown. It may be that the disease starts in the gut or olfactory system (the system which manages our sense of smell), and then spreads along nerve pathways into other areas of the nervous system and brain.
Current treatment
There are several pharmaceutical approaches to treating the symptoms of PD.
- Some therapies focus on replacing the body’s lost dopamine. The drug Levodopa was discovered in the 1960s. It is converted into dopamine in the body, so it acts as a stand-in for the lost dopamine-producing neurons.
- Some other drugs act like dopamine to stimulate the nerve cells in the circuit - these are called dopamine agonists.
- There is a third other major class of drug that works by slowing down the breakdown of dopamine, keeping it in the brain for longer. These are called MAO or COMT inhibitors.
Other drugs can be used to help manage some of the other features of PD, such as constipation, sleep problems, swallowing issues and neuropsychiatric problems including visual hallucinations, acute anxiety, and paranoia.
Patients are also treated with occupational therapy, physiotherapy, healthy diet and exercise. Aerobic exercise, as well as offering generic health benefits and improving physical fitness, shows a trend towards a positive effect on motor symptoms in people with PD.
Surgery, such as deep brain stimulation with implanted electrodes, can be used to treat PD as it gets more advanced, especially when the drugs are working less well. As well as becoming less effective, drugs for PD may begin to produce complications such as excess involuntary movement (so-called levodopa-induced dyskinesias).
These treatments relieve the symptoms of Parkinson's disease, but do not slow down or reverse the damage to nerve cells in the brain. As a result, over time the symptoms get worse, despite treatment. By the time patients are diagnosed with PD, they have often had the disease for years, and have already lost over half of their dopaminergic cells. These cells cannot be restored. Tests that can detect Parkinson’s earlier may help. Scientists are also trying to develop therapies to slow down or stop the disease progression.
How might gene and cell therapies help?
Although the underlying cause of Parkinson's disease is unknown, scientists do know which cell types and which areas of the brain are involved. Researchers are already using stem cells to grow dopamine-producing nerve cells in the lab so that they can study the disease. This is especially useful to understand variations of the disease related to genetic changes the disease when it relates to genetic changes. Because many of the symptoms are caused by the death of a single, well-defined type of brain cell (dopaminergic cells), it may also become possible to treat Parkinson’s by replacing the lost nerve cells with healthy new ones.
Replacing lost cells
Doctors and scientists think that replacing the lost cells, or ‘cell replacement therapy’ may prove successful.
The earliest cell replacement studies for PD were carried out in the 1980s and 1990s. Researchers in Sweden, America and Canada removed developing dopamine-producing cells from foetal brain tissue (the growing substantia nigra). They then transplanted these foetal nerve cells into animals, and later into people with PD, by injecting a solution containing the cells directly into the part of the brain needing the dopamine. Some transplants (or ‘grafts’) led to major improvements in symptoms. Other cases showed slight or no changes.
These small early studies paved the way for larger studies with more participants. However, these studies reported that the transplanted cells might cause side-effects in some participants. These included involuntary movements (graft-induced dyskinesia), which are similar to the levodopa-induced dyskinesia seen in many patients on long-term levodopa treatment. The reason this happens is not yet certain.
Interestingly, looking at the brains of people who had transplants has provided important information about the disease. The transplanted cells have come from very young brains and should not have any ‘clumps’ of the alpha-synuclein protein (or Lewy Bodies). However, when scientists looked at transplanted cells that were less than 20 years old, they could see abnormal alpha-synuclein. Because of this, some scientists believe that abnormal forms of alpha-synuclein may pass from one brain cell to another, causing the disease to spread to other parts of the brain.
One research consortium, TRANSEURO, looked once more at the possibility of transplanting foetal dopaminergic cells. This project aimed to address issues seen in previous studies: not getting the same efficacy in all participants, and graft-induced dyskinesia side effects. The study has finished, and the final results are still awaited as of February 2023. Importantly, the trial has already reported that using foetal tissue was very difficult and they could not get enough cells from the foetal brains to treat the number of patients they planned to. They concluded that dopaminergic cells will need to be produced from stem cells if this treatment is ever to be a therapy for most patients with PD.
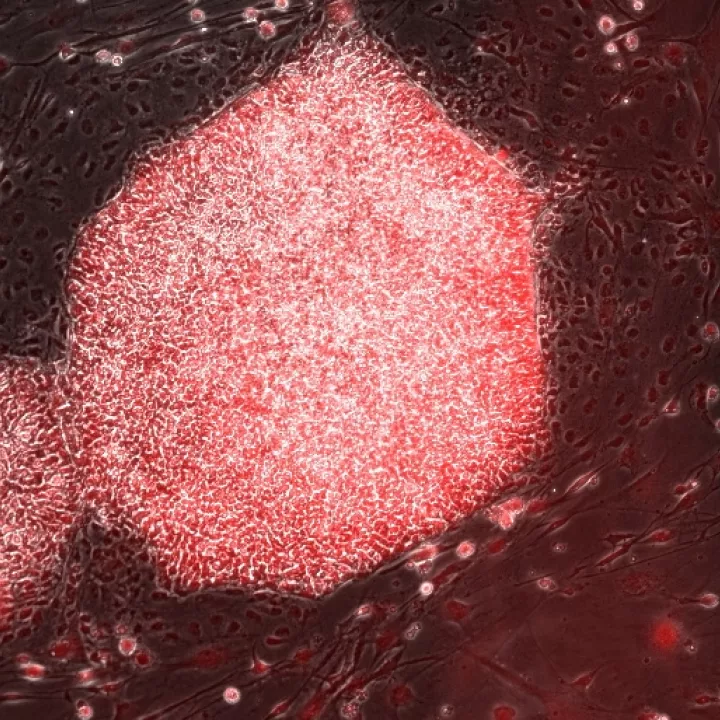
Stem cells are very immature cells that, if given the right chemical instructions, can be guided into becoming the dopaminergic cells needed for transplantation. Learning how to do this at scale has been the focus of a lot of work from many labs. This has now evolved to early clinical trials using two types of stem cells:
- Embryonic stem (ES) cells (stem cells taken from very early embryos), directed to make dopaminergic brain cells, which have now been trialled in patients in New York and soon, hopefully, in Europe.
- Induced pluripotent stem (iPS) cells (made using adult human skin or blood cells in the lab, and then directed to make dopaminergic brain cells). Clinical trials with these type of cells have started in Japan. This type of stem cell could mean that a patients’ own cells could be used for the transplant (so-called autologous transplants). This has been reported with a single patient at time of writing (February 2023) but other trials are planned.
Understanding the disease and developing new drugs
Stem cells also have other uses to help people with PD outside the clinic.
Scientists are making iPS cells from patients with PD, and using these stem cells to produce disease-type brain cells in the lab. These can be used as a powerful tool to study how PD works, and to test substances that could be developed into new drugs to treat the disease.
Gene therapies
There have been three major ways in which gene therapies for PD have been considered.
- Dopamine is made by a series of enzymes in the brain. One gene therapy approach involves injecting the genes for these enzymes into the brain. These genes, wearing the same ‘coat’ as a virus does, then ‘infect’ brain cells, making them produce the missing dopamine like local factories. This has now been the subject of a number of trials including one in France and the UK using a therapy called ProSavin®. The results of these trials have shown some improvements in motor symptoms.
- The second approach is to use gene therapy to regrow dopamine cells, increasing the dopamine they produce. This has been done by injecting the genes for proteins that are known to support the survival and growth of dopaminergic cells act as survival and growth factors (so-called growth factors such as neurturin and GDNF). Modified cells which can produce these proteins can survive, grow, and continue producing dopamine. The results of these trials have been mixed, but are still ongoing. It is still unclear whether they have the power to really stop the dopaminergic cells and the nerve fibres they produce from dying in PD.
- The third strategy is to use a gene therapy to produce a protein (such as an enzyme or some other type of molecule) that is designed to target what might be going fundamentally wrong in the cell. In this way, it would help to slow down or stop the disease. This approach has not yet reached the clinic.
- An emerging new area of research is the idea of ‘direct in situ reprogramming’. This uses a gene therapy technology to directly change the living cells in the brain, transforming them into the cell types that we want (ie., dopaminergic cells). This approach has been successful in cells grown in the lab; by adding a cocktail of genes, glia cells (non-nerve cells which form the brain’s ‘maintenance’ system) can reprogram themselves into dopaminergic nerve cells. This has been more difficult to show in live whole brains in animal models, and is a long way from being tested in the clinic. However, if successful, this technology would avoid the need for cells to be transplanted into the brain, removing the possibility that the patient’s body would ‘reject’ them.
Next steps
Over the next decade we are likely to see the following developments with cell and gene approaches in PD;
- The results from early and current clinical trials, which use dopaminergic cells made from stem cells, may lead to bigger, pharmacy-led trials comparing stem cell therapies to a placebo.
- A new generation of stem cell based dopamine cells will be developed. These will be genetically altered to achieve several different things: to stop them producing alpha synuclein (the protein linked to cell death in PD)
- reduce how visible these cells are to the immune system
- add genetic ‘switches’ in order to regulate how dopamine is released.
- Scientists will continue to research the possibility of direct in situ reprogramming. The ultimate goal of this line of study would be to change patient glia cells (non-nerve cells which form the brain’s ‘maintenance’ system) into functional dopaminergic cells in the body.
- Using stem cells in the lab to model the disease will continue to improve. Instead of a layer of cells lying flat in a dish, 3D ‘organoids’ can be made representing areas of the brain that are affected by disease. These organoids could then be used to rapidly screen for new drugs that might slow or stop the progress of the disease.
- Gene therapies are likely to focus on alleviating specific genetic forms of PD. The gene therapy approaches currently in trials (inducing brain cells to produce extra dopamine, or inducing brain cells to produce more of the substances needed to keep dopaminergic cells alive), help all forms of PD. However, by using gene therapy to correct specific issues, gene therapy could also be used in a more personalised way to treat different genetic forms of PD.
Find out more
Michael J Fox foundation
European Parkinson’s Disease Association
Parkinson’s UK
Cure Parkinson's Trust
World Parkinson Coalition
NECTAR The Network for European CNS Transplantation and Restoration (NECTAR) brings together European groupds working to protecting, repair, and restore the central nervous system. Their social media and website contain updates about research into Parkinson's Disease.