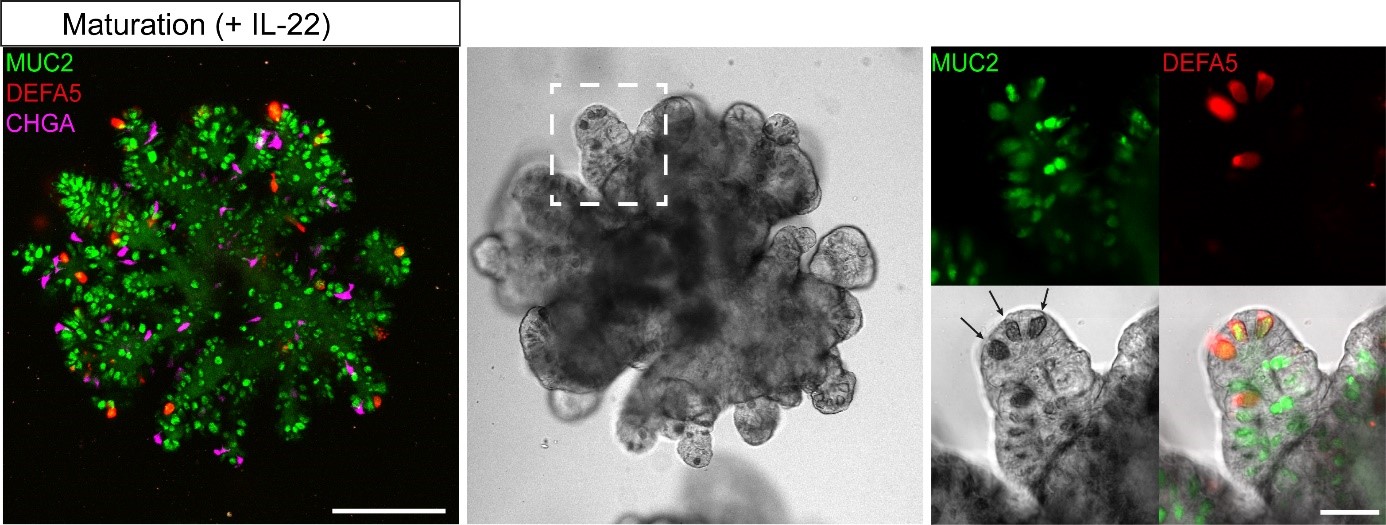
The development of organoids has meant a lot for research on the functioning of human organs and tissues. This has to do with the fact that the mini-organs give a good representation of human biology. However, some of the currently available human organoids, such as the small intestinal organoids, do not yet resemble the original organ fully. Researchers from the Organoid group therefore developed a new, optimised version of the miniature small intestines: organoids that include all cell types of the human small intestine.
Missing Paneth cells
The small intestine contains a wide variety of cells, such as enterocytes, stem cells and Paneth cells. Together, these cells form a barrier between the side where the food passes and the side where the blood vessels and immune cells are. The stem cells in the small intestines continuously create all mature cell types, thereby keeping the barrier in good shape. In particular, Paneth cells are important for preventing infections. They do so by producing antimicrobial peptides that act against harmful bacteria. If active Paneth cells are absent, the small intestine will be more prone to infections. This is a problem in several diseases, among which inflammatory bowel disease (IBD). The previous organoids lacked Paneth cells and did therefore not fully represent healthy human small intestines, while the original mouse organoids described by Toshi Sato in Nature (2009) were complete. This indicated that there was room for improvement of human organoids.
Surprising finding
To induce the formation of Paneth cells in human small intestinal organoids, the researchers studied the effect of various molecules. They discovered that the molecule Interleukin-22 (IL-22) increased the numbers and activity of Paneth cells. The effect of IL-22 on Paneth cells is surprising. Researcher Gui-Wei He explains why: “At the moment, people believe that IL-22 can promote stem cell function. Our study actually showed that IL-22 does not do this, but rather stimulates the activation of Paneth cells.” The discovered function of IL-22 was therefore used to increase the numbers of active Paneth cells in human small intestinal organoids. This led to the development of organoids that mimic healthy small intestines.
Future directions
Now that optimised human small intestinal organoids are available, researchers can expand on what they study. For instance, researchers can use the organoids to make mutations in the DNA of the cells. In this way, they can determine how mutations - occurring in diseases such as IBD - affect the function of the small intestine.
Publication
Optimized human intestinal organoid model reveals interleukin-22-dependency of Paneth cell formation. Gui-Wei He *, Lin Lin *, Jeff DeMartino, Xuan Zheng, Nadzeya Staliarova, Talya Dayton, Harry Begthel, Willine J. van de Wetering, Eduard Bodewes, Jeroen van Zon, Sander Tans, Carmen Lopez-Iglesias, Peter J. Peters, Wei Wu, Daniel Kotlarz, Christoph Klein, Thanasis Margaritis, Frank Holstege, Hans Clevers. Cell Stem Cell, 2022.
*These authors contributed equally