Transplanting donated hepatocytes
Preliminary clinical trials have seen limited success in transplanting donor hepatocytes into a patient’s liver to treat chronic liver disease. However, there are several significant obstacles to this approach.
The attachment and integration (or engraftment) of these new cells into the liver tissue is often very low, due to the harsh environment of the injured liver. Researchers are investigating means of overcoming this issue - for example, by encapsulating donor cells in a protective substance. Another approach being explored is to simultaneously transplant cells which suppress the inflammatory environment, which could potentially reduce the risk of transplant rejection.
Using stem cells to create a supply of cells for transplant
A major barrier to the viability of cell transplants as a therapy for cirrhosis is that it requires large numbers of new cells, which are not readily available. Stem cells, such as induced pluripotent stem cells (iPSCs) or HPCs, combined with new cell culture techniques for growing cells in the lab, could offer significant help in creating enough new hepatocytes for transplants. Using iPSCs to create new hepatocytes may also help avoid attack by the immune system, since iPSCs can be made from cells taken from a patient, such as their skin cells. Researchers are also investigating whether tissue engineering techniques can be used to modify cells for transplant, reducing the risk of immune rejection.
There are still several fundamental questions that must be answered before hepatocyte transplants using stem cells can be used clinically. It will be important to confirm that stem-cell derived hepatocytes are safe for use, and that they function as normal hepatocytes. If these cells are been approved for clinical applications, longer-term studies will need to be carried out to assess the long-term safety and efficacy of their use.
Liver progenitor cells
Researchers have identified liver progenitor cells – precursor cells which can produce new hepatocytes. They are currently undertaking studies to understand how they might be used to both as an investigative tool and to treat patients with chronic liver disease.
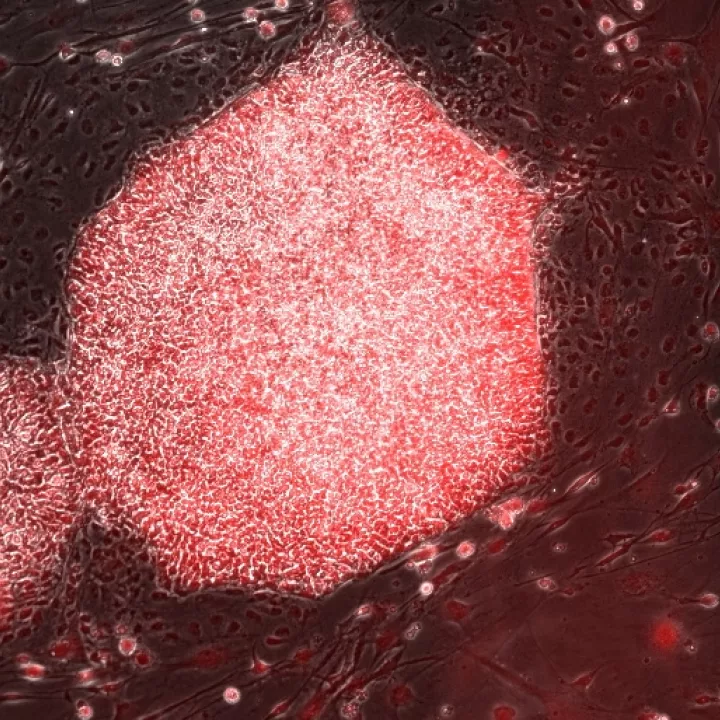
Researchers have established techniques to identify and isolate liver stem cells from donor tissue, and grow them in the lab as ‘organoids’ (three-dimensional, cellular ‘models’ of an organ, which can be grown and maintained in a lab). As a three-dimensional construct, organoids more closely resembles the natural environment in the liver than traditional cell culture. These cells grow rapidly and stably. These organoids can be used to investigate new therapies, as well as to try to recreate and understand the mechanisms of disease. In the longer term, liver progenitor cell organoids may provide a tissue source for clinical transplantation; studies in mice, using human cells, suggests that this is a promising avenue of research.
Using immune cells to change the injured liver environment
Another route to new treatments might be to use cell therapies that target the damaged liver environment to reduce inflammation and scarring, encouraging regeneration of remaining liver tissue. Several types of cells are currently being investigated in clinical trials for this purpose, based on their natural role in the body.
Macrophages are a type of immune cell that ‘clean up’ the dead cells and debris left after an infection or injury. They also promote regeneration. Macrophage therapy is potentially promising to help repair damaged liver tissue. Cells in the blood called ‘monocytes’ (macrophage precursors) can be isolated and treated in the laboratory to produce large quantities of macrophages, which have been shown to have a role in resolving liver scarring. Recent work has shown that macrophages secrete enzymes that break down scar tissue directly, and help remove cells that produce the scar tissue in the first place.
When tested in mice with damaged livers, macrophage therapy showed beneficial roles in both reversing scar formation and promoting liver regeneration. When the amount of scar tissue is reduced, the liver functions better. Human macrophages have been assessed in clinical trials and shown to be safe for use in patients with cirrhosis. They are currently being assessed to determine whether they are effective for improving liver function in patients with cirrhosis, compared to the standard care regime.
Macrophages are an attractive cell therapy because they can be derived from a patient’s own blood cells and therefore would not be rejected by the immune system, as sometimes happens with organ transplants.